What is Soft Tissue Sarcoma in Pets?
soft tissue sarcoma treatment
Soft tissue sarcomas (STS) represent a group of tumors that arise from mesenchymal tissues (including fibrous connective tissue, cartilage, blood vessels, muscles, nerves, or fat). They are histologically distinct, but share many common features; particularly the propensity for local invasion. In the majority of these cases the cause of the tumor is unknown.
Histologic subtypes include: fibrosarcoma, peripheral nerve sheath tumors, malignant fibrous histiocytoma, hemangiopericytoma, and synovial cell sarcoma. Soft tissue sarcomas are relatively common, making up approximately 15% of all skin and subcutaneous cancers in dogs. Soft tissue sarcomas are characterized by having a “pseudocapsule,” poorly defined margins, and fingerlike projections that infiltrate tissue planes (i.e. between muscles and layers of connective tissues). As a result, they tend to be difficult to completely excise, making local recurrence common.
The picture is a typical STS arising from the lateral aspect of the forelimb of a dog. The mass was too large to obtain tumor-free margins with surgery alone, so a combination of surgery and radiation therapy was used. Surgery was performed after a full course of radiation was completed. The patient was cured
In addition to local invasion, they can also metastasize through blood or lymphatic routes. Metastatic rates have been reported from 8-17% in dogs (primarily to the lungs). Histologic grading of STS is based on mitotic rate and necrosis and provides important information with regards to the metastatic potential and survival. For example, grade I and II tumors appear to metastasize in less than 20% of the cases and grade III STS develop metastatic disease in up to 50% of cases. However, biologic behavior can be difficult to predict.
How is STS diagnosed?
Patients most often have a history of a non-painful “lump.” A fine needle aspirate (FNA) is usually performed as a cursory test, but caution must be taken in the interpretation. Soft tissue sarcomas do not exfoliate well (release cells from the mass), so a negative aspirate does not always rule out STS. If an aspirate is suggestive of a mesenchymal tumor, the next step is a biopsy.
For small, easily moveable tumors, an excisional biopsy may be done. For larger tumors, an incisional biopsy is preferred. Wide lateral margins of 3 cm and deep margins of one fascial plane should always be attempted. In one recent study, 100% of local disease control was achieved when deep and lateral margins microscopically were 10 mm (1 cm). Fascial planes tend to act as biologic barriers to local tumor invasion, but this protective effect may be overcome with high-grade lesions.
Staging of STS:
Once a tentative or confirmed diagnosis of STS is made, further testing is necessary to determine if the disease has spread. Thoracic (chest) radiographs, evaluation (FNA) of draining lymph nodes if palpable, and abdominal ultrasound (especially for higher grade tumors) are considered appropriate for routine staging. Immunohistochemistry is recommended for those patients whose tumors are difficult to classify on routine biopsy. This is special staining that provides the pathologist with more information for classification.
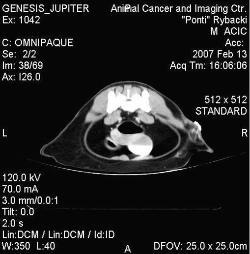
A CT scan from a cat diagnosed with a vaccine associated sarcoma. This patient presented to ACIC after an attempted curative surgery. Radiation was pursued.
In some patients, CT scanning may be necessary to better delineate tumors when attempting to make a decision regarding surgery. Cats with suspected vaccine related sarcomas are routinely scanned prior to treatment due to the locally invasive nature of this disease. If surgery is not considered possible based on the scan, then the scan is used to plan radiation therapy.
Surgery:
For localized disease, wide surgical excision is considered the treatment of choice for STS. Surgery alone can potentially be curative. However, as is the case with most STS that occur on the extremities or where microscopically clean margins are not achieved, further treatment is necessary to prevent local recurrence. If a conservative surgery was initially performed and clean margins not achieved, a second surgery should be performed. If a second surgery is not possible due to the location of the tumor, radiation therapy should be pursued.
This patient underwent radiation therapy for a vaccine associated sarcoma. Cats tolerate radiation with minimal side effects. Hair color changes following radiation therapy are common, but represent only a cosmetic change.
RADIATION THERAPY:
Radiation is a very effective treatment for certain soft tissue sarcomas. It can be used after surgery when margins are considered “dirty” (not tumor free) or can be used to shrink a larger tumor to a point where surgery can be more successful. A combination of surgery and radiation therapy has proven to be effective in keeping patients disease free for extended periods of time.
In one study, 76% of patients were alive and disease free 5 years following radiation therapy of an incompletely excised STS. If radiation is used without surgical intervention (i.e. inoperable), 1 year control rates of 48-67% and 2 year control rates of 33% have been reported.
Chemotherapy:
Most soft tissue sarcomas are locally aggressive and late to metastasize. Chemotherapy is usually reserved for those more aggressive, higher grade tumors, with a known high potential for metastasis. For patients with high grade STS, chemotherapy is recommended, but response rates reported in the literature have been variable. Chemotherapy is most appropriate in the adjunct setting (i.e. used in addition to surgery and/or radiation) rather than as the only form of therapy.
Metronomic Chemotherapy:
This form of chemotherapy utilizes constant exposure to very low dosages of chemotherapy in combination with non-steroidal anti-inflammatory drugs. The goal of this form of therapy is to make the tumors therapeutically controllable by stopping the essential blood supply and nutrients to the tumor. Cancer cells have a higher metabolic rate than ordinary cells and require a continuous supply of oxygen and nutrients. The tumor must build a network of new blood vessels (a process called angiogenesis) in order to obtain the necessary nutrients and oxygen it needs to survive.
In human medical research, a lot of emphasis has been placed on the study of angiogenesis and novel therapies to target it (i.e. stop angiogenesis of tumors). In a recent study in veterinary medicine, patients with STS that were incompletely excised, but did not undergo radiation, and were treated with metronomic therapy alone showed significantly improved survival rates when compared to patients that received no further treatment after surgery. Therefore, the use of metronomic therapy alone or in combination with other forms of therapy may gain more popularity in the future.